We’re emerging from lockdown! Whilst things are far from usual I’m now back seeing patients again. The sun is shining and all things knee are moving forwards.

Four months post op slightly reminds me of emerging from the first few months of motherhood. It does get easier! The differences between ACL journeys can also be just as diverse as raising kids. If you’re struggling you aren’t alone, likewise if things are going great & you’re returning to running & into plyometrics that’s equally great.
Just like any other challenge, surround yourself with support from people that are helping make that journey positive. Get in touch if you want some advice, motivation or just to swap stories.
I did start with a treadmill jog in recent weeks as impact loading assessment more than anything else. 5mins walk, 1 min jog, 5mins walk 30secs. This session did build a bit of confidence but did feel “odd” & that was enough for my patella-femoral joint at the moment which is irritable.
I made it back to physio myself this week & it was great to be back on the Alter-G for some work towards running. I started with backward walking, followed by forward fast walk. I jogged for 7 mins with 60% of body weight taken off. That’s the baseline at the moment. It’s useful (compared to my 1min on treadmill) to get more time in running whilst analysing & working on gait with less impact. You get feedback on stride length, weight distribution, time in stance phase & can change things. Hopefully when I get back to full weight bearing I will be as near even gait pattern as possible and will have gradually built up tolerance to loading. Hopefully this will limit me reinforcing suboptimal movement patterns and stop any longer term issues from picking up bad habits.
One example is my heel kick. On the Alter G, I could see from the rear camera I wasn’t pulling up my right heel as high as the left, probably because my hamstring isn’t working as hard on the operated leg where the graft was taken. A quick correction & I could see in real time things change.
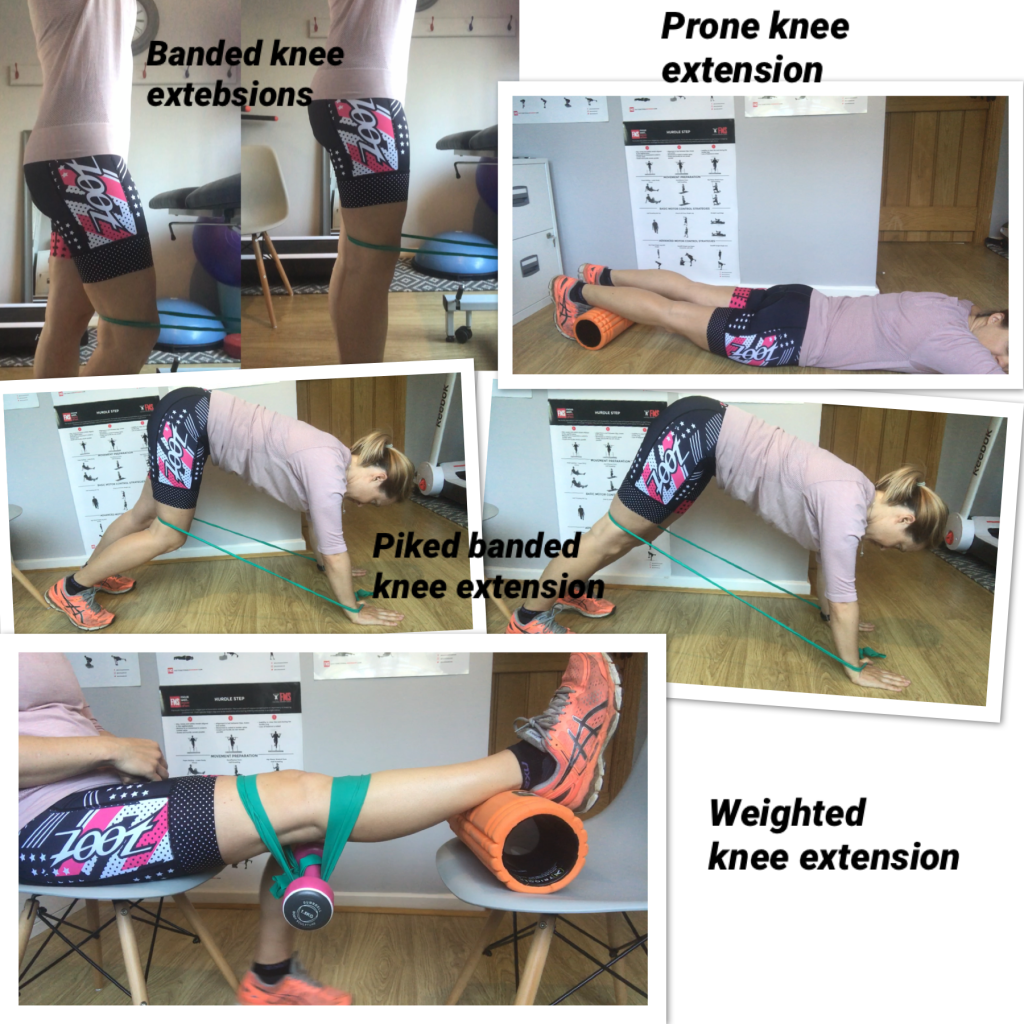
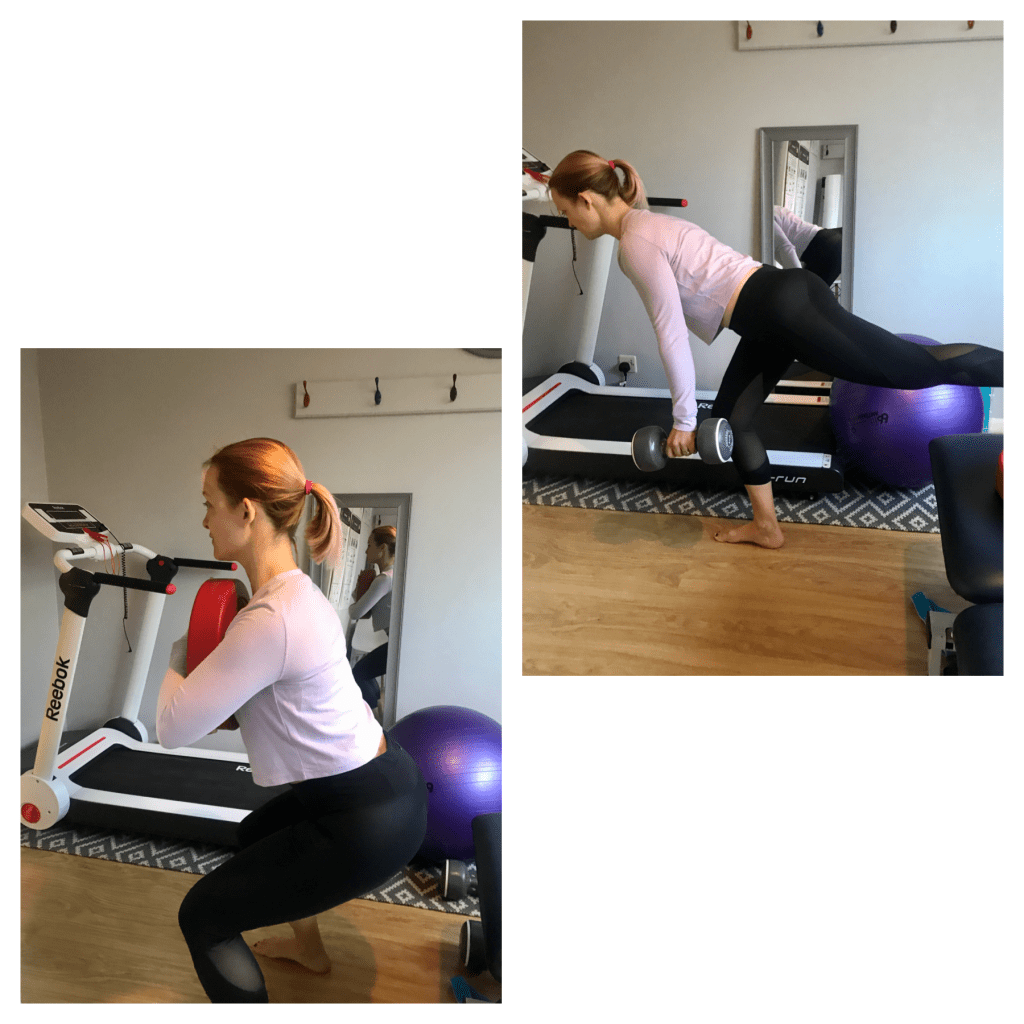
Strength work continues to progress. I’ve now introduced some low level plyometrics (jumping type activities) into my rehab and added in some variation too. I’ve been outside on the mountain bike but am not ready for the road bike outside yet. It’s a standard environment in the house with no traffic & limited opportunities to fall off! I can also pull my foot out of the shoe instead of the twisting motion of uncleating. I have started using cleats on the turbo trainer which is a game changer. I also did my first interval ride on Zwift & was promptly dropped by the group! Great to be adding some different workouts in though. Variety in rehab keeps things slightly more interesting!

Another training variation was the addition of a stand up paddle board. It is soooo nice to finally (6 months after the injury) to be a bit active outside & it’s great for balance training. I would say if you are thinking about getting on a SUP, go in flat & deep water in these relatively early months. Keeping any excited kids well clear of capsizing the board means you have the perfect opportunity for some alone time too!! The potential risk of injury to the ACL graft could come from a slip & twist off the board or landing awkwardly if you fall off in shallow water. If in doubt check with your physiotherapist before you head out.

A few of the plyometric exercises I have added in are below. As you will see I have plenty to work to do & compensations to iron out. There are a plethora of exercises that you can be doing at 4 months post op depending on how your rehab is progressing. Get in touch if you need some ideas.
Hopefully your personal rehab is heading in the right direction & you are starting to see the benefits of the work you are putting in. Stick with it….